Hernia Mesh Removal
Hernia mesh removal may require a rebuild of the abdominal wall. The procedure can safely be performed by specialized hernia surgeons using open, laparoscopic or robotic surgery. Complications requiring hernia mesh removal include chronic pain, infections and hernia recurrence.
Surgeons repair about 90 percent of hernias with mesh — a net-like implant that bolsters weak tissue and supports organs. The majority of patients do well, but an increasing number suffer mesh-related complications that require hernia mesh removal surgery.
Recurrence was the most common complication before the hernia mesh’s invention. Research is mixed on how long a mesh hernia repair will last. A 2022 study followed 100 patients for ten years after a ventral abdominal hernia repair.
No recurrence was recorded after three years, while about 10% had a recurrence after roughly eight years. Two patients had a central breakdown of the mesh at about seven years. Mesh had stretched across the defect by an average of 21%. Mechanical testing showed that the mesh lost its elasticity at low forces.
One of the first doctors in the United States to remove hernia mesh was Dr. Kevin Petersen, a surgeon in Las Vegas. In 1995, he met a patient with disabling groin pain. Petersen found mesh in the location of the patient’s pain.
“I told the patient that the mesh was likely causing his pain and that, although it had not been done before, he needed his mesh removed,” Petersen told General Surgery News in 2015.
“We are seeing a surge in the number of patients who are seeking to have their mesh removed.”
The patient’s pain was resolved after Petersen performed a hernia mesh removal operation. Studies show the majority of patients with mesh-related complications who have their mesh removed experience an improvement in symptoms — especially pain.
Researchers don’t have an exact figure for the number of patients who require mesh removal surgery due to complications, but the numbers are increasing.
“We are seeing a surge in the number of patients who are seeking to have their mesh removed. This is reflected not only in our clinical practice, but also in lay discussions in online forums and social media,” said the authors of a 2019 article published in Journal of the American College of Surgeons.
Why Surgeons Remove Mesh
Certain hernia mesh complications require removal of the mesh itself. One of the most common reasons for mesh removal is severe hernia mesh pain.
- Adhesions (scars that cause tissues or organs to stick together)
- Hernia recurrence
- Infection
- Intestinal blockages
- Mesh displacement (movement through the abdominal cavity)
- Mesh erosion into organs
- Meshoma (wrinkling of the mesh that causes pain or hernia recurrence)
- Nerve entrapment or damage
- Rejection of the mesh implant
Dr. Shirin Towfigh and colleagues at the Beverly Hills Hernia Center performed 105 mesh removals over four and a half years, according to a study in Hernia.
Over that period, researchers in the study found that the most common indication for abdominal mesh removal was infection, and mesh was removed from the abdomen of females more often than males.

Doctors removed mesh from the pelvis more often in men, and the most common reason for removal in the pelvis was pain.
Symptoms of complications that require mesh removal include fever, problems urinating or blood loss, leakage or severe swelling at the surgery site.
What Is the Procedure Like?
Hernia mesh removal surgery is similar to the initial hernia repair surgery but can be more complicated. For example, removal may require a rebuild of the abdominal wall. Depending on the type of mesh used, surgeons may need to remove all or part of the mesh and the tacks that held the old mesh in place.
In some cases, surgeons may have to reinsert another piece of mesh if damaged tissue cannot prevent hernia recurrence.
On average, the surgery takes about an hour to an hour and a half. Most patients who have mesh removed require general anesthesia, and some will require a hospital stay of at least one day.
Recovery may take several weeks or months, depending on the extent of the surgery. Patients should ask their doctor about what to expect.
The three main surgical techniques for mesh removal are open, laparoscopic and robotic.
| Surgery Type | Pros | Cons |
|---|---|---|
| Open | Lower cost, shorter operation time, option to use local anesthesia | Longer recovery time, more post-op pain |
| Laparoscopic | Shorter recovery time (days versus weeks), smaller incisions, less blood loss | More challenging technique; potential to harm nearby blood vessels, bladder and other organs; higher cost than open surgery; longer operation time |
| Robotic | Shorter recovery time, smaller incisions, less blood loss, possibly fewer complications than laparoscopic surgery | Only highly skilled surgeons should perform these surgeries, more expensive than laparoscopic surgery, significantly longer operation time than laparoscopic surgery |
Traditional or Open Surgery
Before surgery, doctors may prescribe medication to help patients relax. During the surgery, depending on the size of the mesh and the complexity of the procedure, doctors may choose general or local anesthesia.
In open surgery, or traditional surgery, the surgeon makes an incision where the mesh is located and feels around the area for the mesh. They then cut around the surrounding tissues and nerves to remove the mesh, reconstructing the abdominal wall afterward if necessary.
This type of surgery requires larger incisions and more cuts in muscles and tissues. Recovery time is generally several weeks.
Laparoscopic or Minimally Invasive Surgery
Laparoscopic surgery, or minimally invasive surgery, requires three small incisions in the abdomen. Unlike open surgery, this type of procedure always requires general anesthesia, which has additional risks.
Laparoscopic surgery is a complex procedure, and risks include damage to blood vessels, nerves, the bladder and the spermatic cord, according to Erfan Zarrinkhoo and Dr. Shirin Towfigh of the Beverly Hills Hernia Center.
“Laparoscopic mesh removal after inguinal hernia repair with mesh is considered to be complex and poses risk for very serious complications.”
During the procedure, the abdomen is inflated with gas and a camera is passed in through the belly button. Surgical instruments are inserted through the other small incisions, allowing the surgeon to carefully cut the mesh out and avoid damage to other structures.
This type of surgery takes longer than open surgery but is associated with less blood loss and a faster recovery time — days instead of weeks, in some cases.
Researchers in the Netherlands studied 14 patients who had laparoscopic mesh removal surgery and reported their findings in a study published in Surgical Endoscopy. The patients experienced no complications during or after surgery and reported a decrease in pain following the procedure.
“Eight months postoperatively (median), pain scores had dropped from eight to four. Satisfaction was good or excellent in ten patients,” authors said.
Robotic Surgery
Robotic surgery is like laparoscopic surgery — performed with small incisions, a camera, general anesthesia and inflation of the abdomen — but instead of standing near the patient, the surgeon sits at a console to control a robot positioned next to the patient. To perform the surgery, the doctor watches three-dimensional images of the inside of the abdomen. This allows the surgeon to see the structures more clearly and potentially avoid injuring the surrounding tissues, organs and blood vessels.
Surgeons at the Beverly Hills Hernia Center compared laparoscopic and robotic mesh removal in 25 patients undergoing hernia mesh revision surgery. Study authors Erfan Zarrinkhoo and Dr. Shirin Towfigh found robotic surgery to have fewer complications than laparoscopic surgery, where the risks typically include spermatic cord injury, nerve injury and blood vessel injury.
They concluded robotic-assisted surgery may decrease laparoscopic surgery risks.

Robotic surgery requires a highly skilled surgeon and has a much longer operative time than laparoscopic surgery. It also costs more.
In addition, it has its own unique complications.
Risks and Benefits of Removing Mesh
Like other surgical procedures, hernia mesh removal has risks. There are also no guarantees that mesh pain will go away.
According to the Shouldice Hospital in Ontario, Canada, pain worsened after mesh removal in only 2 percent of cases. The hospital performs mesh removal surgeries and also repairs hernias without the use of mesh.
“Early experience believes that these unfortunate cases [of worsening pain after mesh removal] are due to the impossibility of removing the entire mesh, which may have become too adherent, penetrated major blood vessels or infiltrated organs,” according to the Shouldice Hospital website.
Before patients undergo a mesh removal procedure, they should discuss the benefits and potential risks with their doctor. For emergencies such as infection or bowel obstruction, surgery is necessary. But in cases of pain, surgeons may recommend more conservative pain management options.
- Adhesions (scars that cause tissues or organs to stick together)
- Bleeding and infection
- Numbness
- Ongoing groin pain
- Ongoing systemic symptoms
- Recurrent or new hernia formation
- Small and large bowel obstruction
- Testicular pain
- Injury to major organs and blood vessels in the abdomen
For some patients with severe chronic pain, the benefits of surgery may outweigh the risks.
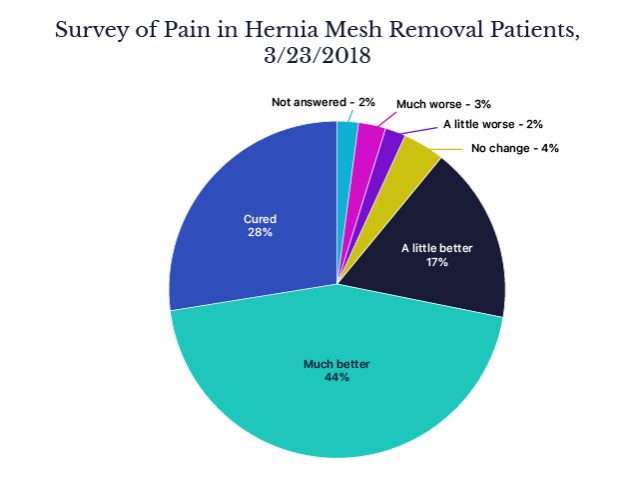
According to reports from Shouldice Hospital, over 90 percent of their patients have improvement in pain after mesh removal.
Dr. Kevin Petersen followed his patients after mesh removal and presented his findings at the World Conference on Abdominal Wall Hernia Surgery in 2015 in Milan, Italy. About 80 percent of his patients experienced significant or complete improvement of pain.
Compensation for Removal and Revision Surgery
Patients who have had to undergo hernia mesh removal surgery often suffer from financial and emotional losses.
Some have had to live with crippling pain that causes them to lose their jobs and live on disability, like the mesh patient who sought help from Dr. Kevin Petersen in 1995.
People who have had mesh removal or revision surgery may be entitled to compensation for lost wages, medical bills and pain and suffering caused by faulty mesh products.
Thousands of patients have filed hernia mesh lawsuits against Atrium, Bard Davol, Covidien and Johnson & Johnson’s Ethicon unit. Bard Davol paid out $184 million in 2011 to patients who suffered complications from its Kugel Patch.
Lawyers recommend that patients tell their surgeons to preserve the hernia mesh after removal surgery.
Calling this number connects you with a Drugwatch representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.




