Benicar Side Effects
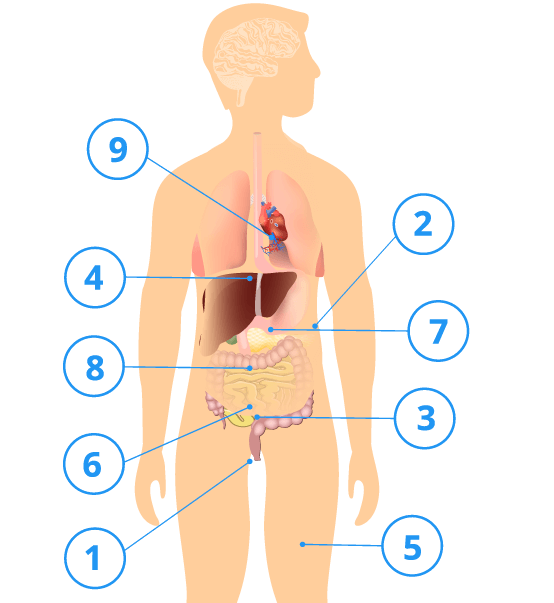
A common Benicar (olmesartan medoxomil) side effect is dizziness. Serious side effects include fetal toxicity in pregnant women and sprue-like enteropathy, a gastrointestinal condition similar to celiac disease that can lead to weight loss, malnutrition, severe diarrhea and hospitalization.
According to the U.S. Food and Drug Administration Adverse Event Reporting System, known as FAERS, brand names Benicar and Benicar HCT and their generics led to 16,845 adverse events from 2002 to September 30, 2019. Of those reports, 12,975 were serious, including 596 deaths.
FAERS reports are voluntary and the FDA does not verify if the drugs actually caused these side effects. The most reported adverse events include sprue-like enteropathy, gastroesophageal reflux disease, diarrhea, weight loss and acute kidney injury.
The drug’s label has a black box warning for fetal toxicity. Pregnant women should not take the drug. Women should stop taking the drug if they find out they are pregnant.
Benicar can also cause some less severe but still serious conditions that require continued monitoring. Patients with dehydration and low sodium levels may experience low blood pressure after starting the drug. People with severe congestive heart failure or who are otherwise susceptible may suffer impaired kidney function. There’s also a risk of electrolyte imbalances, including elevated levels of potassium in the blood serum. Facial swelling (or edema) occurred in 5 patients out of 3825 patients in clinical studies.
Benicar’s package insert says dizziness was the most common side effect in clinical trials. It occurred in about 3 percent of trial participants. Benicar HCT’s most common side effects include nausea, hyperuricemia, dizziness and upper respiratory infection. These occurred in 2 percent or more of trial participants.
According to the insert, there were several post-marketing reports of adverse reactions linked to Benicar. But researchers cannot say how often these occur or if the drug caused them.
- Acute renal failure
- Alopecia (hair loss)
- Anaphylactic (serious allergic) reactions
- Angioedema (swelling under the skin)
- Asthenia (decreased muscle strength)
- Hyperkalemia (high levels of potassium)
- Increased blood creatinine levels
- Pruritus (itching of the skin)
- Rhabdomyolysis (muscle tissue breakdown)
- Sprue-like enteropathy (gastrointestinal problems)
- Urticaria (rash)
- Vomiting
Fetal Toxicity
Research has linked olmesartan, the active ingredient in Benicar, to fetal toxicity. The effects on the fetus typically happen when women take the drug during the second and third trimester of pregnancy.
The package insert says use of the drug during the second and third trimester of pregnancy reduces fetal function and increases fetal and neonatal disease rates and death.
The drug can also harm amniotic fluid, which can be associated with underdeveloped fetal lungs and deformed bones, including the skull. Other fetal complications include urine retention and low blood pressure.
Women who become pregnant are advised to discontinue the medication as soon as possible in consultation with their doctors. If a pregnant woman must continue taking the drug, she should be advised of the potential risk to her fetus.
The manufacturer says it doesn’t know if the drug is excreted in human milk, but it has been found in low concentrations in the milk of lactating rats. Because of the potential for adverse effects on infants, nursing mothers should consult with their doctors about whether to continue taking the medication. Children younger than 1 year should not ingest the drug because it may alter normal kidney development.
Severe Gastrointestinal Side Effects
In 2013, the U.S. Food and Drug Administration issued a safety announcement warning consumers that Benicar, as well as similar drugs such as Benicar HCT, Azor, Tribenzor and generic versions, can cause severe intestinal complications collectively known as sprue-like enteropathy.
Most often, when patients take prescription medications that cause diarrhea the side effect occurs without permanent damage to the intestines. But sometimes severe diarrhea can cause substantial weight loss, malabsorption and permanent damage to the intestines. These symptoms are typically associated with celiac disease due to gluten exposure. However, drug-induced enteropathy can occur independent of gluten intake and does not go away with a gluten-free diet.
The FDA evaluated reports in published literature as well as databases including the FDA’s Adverse Event Reporting System (FAERS), the Centers for Medicare and Medicaid Services (CMS) database and a pilot version of a national medical product monitoring system called Sentinel Initiative.
“FDA’s evaluation found clear evidence of an association between olmesartan and sprue-like enteropathy,” the agency said.
The gastrointestinal disorder usually resolved once patients stopped taking the drugs, according to the FDA. In severe cases, patients ended up in the hospital. Some suffered from villous atrophy, which occurs when microscopic, finger-like projections that help absorb nutrients erode away, causing the walls of the small intestine to essentially become a flat surface. This can cause serious nutritional deficiencies. This condition also resolved in most patients when Benicar was discontinued.
Based on its findings, the FDA approved changes to the drugs’ labels to include sprue-like enteropathy. More than 2,000 people who used Benicar and developed intestinal side effects filed lawsuits.
In November 2017, the consumer advocacy group Public Citizen petitioned the FDA to remove Benicar from the market and ban the sale of the drug and several generic versions because of “overwhelming evidence” that the medications cause sprue-like enteropathy. The group noted that the risk of the life-threatening gastrointestinal disorder is “far greater” with olmesartan than with other medications in the same class of drugs.
The FDA responded to the petition in October 2019. The agency denied the petition to withdraw Benicar from the market as no new evidence regarding the drug’s safety was reported.
According to the FDA response, the finding from the studies cited in the petition were adequately addressed in the drug labeling change in 2013. With respect to the risk of the disorder being greater than other medications in its class, the FDA stated that education of the patient and healthcare provider to monitor for symptoms of this potential adverse event addresses the concern.
Furthermore, the FDA’s response stated that withdrawal of this agent from the market would adversely impact a large number of patients who have adequate blood pressure control without adverse events with Benicar and Benicar-containing medications. The FDA concluded with the statement that the safety of the drug would continue to be under surveillance.
Causes and Symptoms of Olmesartan-Induced Sprue-Like Enteropathy
Drug-induced diarrhea can occur for any number of reasons. Its cause is uncertain in patients taking Benicar. However, the FDA wrote that research suggests olmesartan-induced sprue-like enteropathy may be a delayed hypersensitivity or immune response to the medication because it develops months to years after starting treatment.
Signs and symptoms of sprue-like enteropathy
- Severe, chronic diarrhea
- Substantial weight loss
- Malabsorption
- Abdominal pain
- Fatigue
- Bloating
- Nausea
- Vomiting
- Anemia
Patients experiencing olmesartan-induced sprue-like enteropathy exhibit signs and symptoms similar to individuals suffering from celiac disease.
In one 2022 case study, a man suffered from persistent watery diarrhea 10 times a day for 60 days before doctors diagnosed him with olmesartan‐related sprue‐like enteropathy. Researchers found the drug had caused damage to his intestines. After discontinuing Benicar, the tissue began to heal.
The FDA advises patients to contact their physicians if they develop severe, chronic diarrhea or significant weight loss while taking Benicar, even if it takes months or years for the symptoms to appear. If a doctor cannot identify causes other than the medication, then he or she may recommend discontinuing the drug and replacing it with another blood pressure treatment.
Calling this number connects you with a Drugwatch representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


