EVALI
EVALI is an acronym that stands for e-cigarette or vaping product-use associated lung injury. The U.S. Centers for Disease Control and Prevention identified and named the condition in 2019 amid a nationwide outbreak of vaping-related injuries. In early research, doctors at the Mayo Clinic described it as resembling a chemical burn to the lungs.
EVALI is a serious and sometimes fatal lung injury related to vaping. An outbreak of EVALI in 2019 led to hundreds of hospitalizations and dozens of deaths. The CDC has said vitamin E acetate, an ingredient sometimes used in THC-based vape fluids, is “strongly linked” to the condition. THC is the chemical that causes most of marijuana’s psychological effects. Symptoms of EVALI can include problems related to breathing or to the digestive system.
The severity of EVALI has led many patients or their survivors to file e-cigarette lawsuits as part of a growing mass litigation in federal court.
A Brief History of EVALI
Health care workers started noticing mysterious vaping-related lung injuries in March 2019 but didn’t see a connection at first. Doctors at Children’s Hospital of Wisconsin were among the first to notice a pattern after three teens showed up with the same symptoms over the July Fourth weekend.
X-rays showed interstitial pneumonia, a type of pneumonia that crisscrosses the entire lung and is associated with serious underlying diseases. Two other teens had shown up at the hospital with the same symptoms just weeks earlier. All the teens told doctors they had recently used e-cigarettes.
After health care workers in Wisconsin went public with the discovery, state and federal public health agencies launched investigations into the outbreak. Cases were eventually identified in all 50 states, the District of Columbia and two U.S. territories – Puerto Rico and the Virgin Islands.
The CDC and state health departments created case definitions to classify confirmed and probable cases in a consistent manner.
The outbreak peaked in September 2019, and began a gradual decline. But the CDC continued to receive reports of new cases into 2020. As of Feb. 18, 2020, EVALI had caused 2,807 hospitalizations and resulted in 68 deaths in the United States and its territories, according to the CDC. There has been no new information from the CDC as of November 2022.
However, the California Department of Public Health reported a total of 249 cases and five deaths in October 2022.
| Under 18 | 15% |
| 18 to 24 | 37% |
| 25 to 34 | 24% |
| 35 and Older | 24% |
The agency calculated the median age of those hospitalized as 24 and reported that 76 percent of patients were between 18 and 34 years old. Patients as young as 13 have been diagnosed with EVALI. The youngest to die from it was 15. The information was based on data gathered as of Jan. 14, 2020, according to the CDC.
The cases reported to the CDC included those that had happened prior to the outbreak. But the agency did not say at the time how far back the cases went. In September 2019, Bloomberg reported that it discovered at least 15 vaping-related lung injuries reported in medical literature prior to the outbreak. Those cases went back to 2011.
Virginia doctors in a 2016 case study named an e-cig user’s condition “vapor lung,” according to the Bloomberg report. Other names used to describe EVALI before the CDC coined the term have included VAPI (vaping associated pulmonary injury), vaping-associated lung injury, vaping-associated lung disease, and vaping-induced lung injury.
Symptoms
EVALI quickly became the most serious e-cigarette side effect, but it can be difficult to diagnose.
It may be mistaken for the flu because many of the symptoms are similar. EVALI cannot be distinguished from influenza or other respiratory conditions based on signs, symptoms, a doctor’s examination or most basic tests by themselves. But it can quickly develop into a potentially deadly lung injury if not treated.
It is important for people who believe they may have EVALI to let their doctor know about their vaping habits. This includes telling the doctor about all THC and nicotine vape fluids the patient has recently used as well as where they were obtained.
- Abdominal pain
- Chest pain
- Chills
- Cough
- Diarrhea
- Fever
- Nausea
- Shortness of breath
- Stomach pain
- Vomiting
- Weight loss
Source: Centers for Disease Control and Prevention
Diagnosis
Diagnosing EVALI requires doctors to eliminate other possible causes of a patient’s symptoms. The doctor begins with an examination and questions about e-cigarette use to determine the patient’s risk for EVALI.
The doctor will perform a pulse oximetry test, a painless measurement to determine how well oxygen is being carried to parts of the body farthest from the heart. Patients with low oxygen levels may require a chest x-ray to check for lung damage.

Source: Wikipedia
A chest x-ray may also be considered for patients exhibiting respiratory or gastrointestinal symptoms. The doctor will attempt to rule out viral or bacterial pneumonia based on those x-rays.
What Causes EVALI?
Vitamin E acetate is “strongly linked” to the EVALI outbreak, according to the CDC. But the agency has not ruled out other vaping chemicals as potential causes. Vitamin E acetate is sometimes used as a thickening agent in vape liquids.
Vitamin E is found in a wide variety of foods and is used in dietary supplements and cosmetics. It’s generally safe to eat, swallow or to apply to the skin. But research has shown that it can interfere with lung functions if it’s inhaled.
A 2020 study in The New England Journal of Medicine looked at medical samples from 51 EVALI cases and found vitamin E acetate in 48 of the patients.
Other chemicals examined in the study included plant oils, coconut oil and other medium chain triglyceride oils, petroleum products and other thickening agents. The only other chemicals found in any of the patients were coconut oil and limonene. Those turned up in one patient each.
Both THC and Nicotine Vape Liquids Have Been Linked to EVALI
EVALI cases have been identified in people who only vaped nicotine or THC liquids exclusively. But THC users were more likely to be diagnosed with EVALI in a CDC analysis.
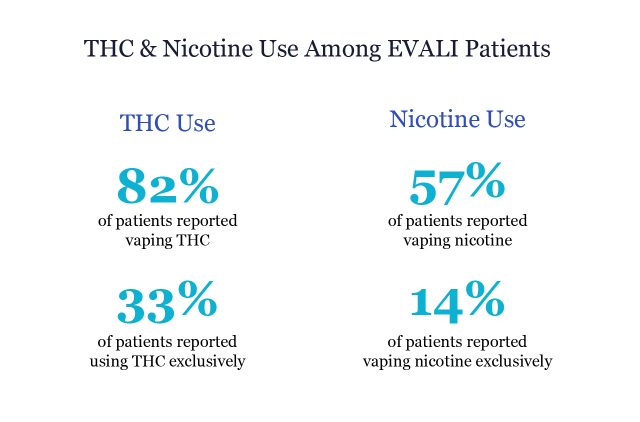
Of 2,022 patients hospitalized for EVALI as of Jan. 14, 2020, 33 percent reported vaping only THC liquids according to the CDC. Another 14 percent said they vaped only nicotine products. Overall, 82 percent of the EVALI patients in the analysis reported using THC products, either exclusively or along with nicotine vape products.
Treatment and Prevention
Doctors may first prescribe antibiotics or antiviral drugs to rule out possible infection in suspected EVALI cases. Patients also receive corticosteroids to reduce inflammation in the lungs. But 96 percent of the people who develop EVALI require hospitalization, according to the American Lung Association. Once hospitalized, many patients require a mechanical ventilator to help them breathe.
At least one EVALI patient, a 17-year-old boy, required a double lung transplant due to irreparable vaping-related injuries. Without the new lungs, the teen “would have faced certain death” according to Dr. Hassan Nemeh who led the transplant team at Detroit’s Henry Ford Hospital.
Prior to the transplant, the teen spent a month hooked to an ECMO machine, which delivered oxygen directly to his blood and supported his heart and lung functions.
There have been reports of people relapsing or even dying from EVALI shortly after their release from the hospital. It’s recommended that patients have a follow-up appointment with their doctors within 48 hours of leaving the hospital.
Preventing EVALI
The best way to prevent EVALI is to avoid vaping products, according to public health organizations.
The U.S. Food and Drug Administration and the CDC recommend that people avoid using any vape products containing THC. The agencies stress that products obtained from informal sources, such as family, friends and online dealers should particularly be avoided.
The agencies also recommend that people should not add any additional substances to vape fluids. The FDA urges people who choose to continue vaping to monitor themselves for EVALI symptoms and seek medical attention if they have health concerns.
People who have stopped smoking tobacco after taking up vaping should not return to tobacco products, according to the CDC. The agency instead recommends seeking medical advice on ways to quit smoking.
E-cigarettes and other vaping products have not been approved as smoking cessation devices. The CDC recommends that anyone considering e-cigarettes should instead talk to their health care professional about FDA-approved smoking cessation options. These include prescription and over-the-counter medications.
The CDC recommends that people who have not started smoking or vaping avoid both. Young people and pregnant women should not vape under any circumstance.
New Vaping Regulations
The 2019 EVALI outbreak focused new attention on vaping’s hidden dangers, shining a light on a nearly decade-long delay in aggressively regulating the vaping industry.
“EVALI triggered a great deal of regulatory and legislative attention,” Dr. Robert Jackler, co-founder of Stanford Research into the Impact of Tobacco Advertising, told Drugwatch. “EVALI is trivial compared to the long-term mortality and morbidity of smoking. But EVALI did focus the public’s attention on the consequences of vaping.”
There were few regulations on the vaping industry during its first 10 years. But by the height of the outbreak, the FDA renewed scrutiny on the vaping products while states and cities proposed or enacted e-cigarette and Juul bans.

Source: KQED
“I think if there had been better regulation of e-cigarettes, we wouldn’t have seen as many cases,” Dr. Joshua Mansour, a Los Angeles-based hematologist and oncologist, told Drugwatch. “When something like vaping is regulated, it’s harder for people to get, harder for children to get. That definitely plays a role in decreasing the likelihood of patients being hospitalized.”
Calling this number connects you with a Drugwatch representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.




