Pradaxa Side Effects
Patients who take the blood thinner Pradaxa (dabigatran etexilate) are at risk for serious, uncontrolled bleeding. This can be fatal. Other potential serious side effects include heart attack and liver damage. More common ones include stomach pain and indigestion.
Pradaxa side effects range from indigestion to life-threatening, uncontrolled bleeding. The U.S. Food and Drug Administration warns that taking the drug may cause patients to bruise more easily. It may take longer for any bleeding to stop while using the drug, the agency says.
The FDA also requires a black box warning about spinal/epidural hematomas and dangers associated with stopping the medication.
Pradaxa was the most frequently mentioned drug in the FDA database of adverse event reports in 2011. This means the drug was associated with injuries that resulted in prolonged hospitalization, disability or death. Aside from bleeding, other adverse events have included acute kidney failure, strokes and possible liver failure.
The Institute for Safe Medication Practices looked at adverse event reports again in 2015. The blood thinner continued to have the largest number of overall serious reports in the U.S. It also had the largest total number of reported severe hemorrhages (bleeds) and the most patient deaths.
Common Side Effects and Allergic Reaction
Pradaxa’s maker lists the drug’s common side effects as indigestion, upset stomach, burning and stomach pain. It also warns that some patients who use the drug may develop allergic symptoms.
Patients should tell their doctor if they experience any of these side effects or if the side effects don’t go away. They should get medical help right away if they notice any of the symptoms of an allergic reaction.
- Chest pains or tightness
- Swelling of the face or tongue
- Difficulty breathing or wheezing
- Feeling dizzy or faint
Bleeding Risks
Bleeding is the most frequently reported Pradaxa side effect. The body usually stops itself from losing too much blood by forming clots, but Pradaxa reduces the body’s ability to do so. As a result, people may notice they bruise more easily and it may take longer for bleeding to stop when they suffer a cut or injury.
As with other blood thinners, Pradaxa can also cause significant and sometimes fatal bleeds. The drug also interacts with other medications, including common painkillers, in ways that can increase this risk.
Taking Pradaxa with other drugs may increase the risk of bleeding. For example, one 2022 study, researchers found an increased risk or bleeding when patients took Pradaxa with flucanozole, an antifungal also known as Diflucan.
Signs and symptoms of serious bleeding can include:
- Joint pain, swelling or discomfort joint
- Headaches
- Dizziness or weakness
- Recurrent nose bleeds
- Bruises that happen without a known cause or that get larger
- Bleeding from a cut that is severe and can’t be controlled
- Unusual gum bleeding
- Heavier than usual menstrual or vaginal bleeding
- Pink or brown urine
- Red or black stools (looks like tar)
- Coughing up blood or blood clots
- Vomiting blood or vomit that looks like coffee grounds
Dr. Alan Jacobson, the director of anticoagulation services at the Veterans Administration (VA) health care system in Loma Linda, California, told Reuters that the “average patient” may not understand all the drug’s contraindications and may be unaware of interactions with other medications.
FDA Reports Increased Risk of GI Bleeds
Using Pradaxa increases the risk of major gastrointestinal hemorrhaging. In a major trial, gastrointestinal bleeds were reported at a rate of 1.59% a year, meaning 1.5 out of every 10 patients taking Pradaxa experienced a stomach bleed.
In May 2014, the FDA alerted the public that the risk is higher with Pradaxa than warfarin. The announcement came following a new study that included information from more than 134,000 Medicare patients older than 64.
In another study, researchers looked at two reported cases of severe rectal bleeding in patients taking the drug. One was a 79-year-old woman who was admitted to the hospital two months after she started the medication. The other was an 84-year-old man. Both took 110 mg of the medicine twice daily to treat chronic atrial fibrillation.
“In both cases, an objective causality assessment revealed that those adverse reactions were probably related to dabigatran etexilate,” the researchers wrote.
The peer-reviewed journal Annals of Pharmacotherapy published the findings in June 2012.
Other gastrointestinal adverse reactions in clinical trials included: abdominal pain, gastroesophageal reflux disease (GERD), esophagitis, erosive gastritis, stomach bleeding and ulcers.
Brain Bleeds and Risk Factors
Hemorrhages in the brain and central nervous system caused by Pradaxa can be as harmful as a stroke. Researchers say brain bleeds are the most devastating complication of blood thinners.
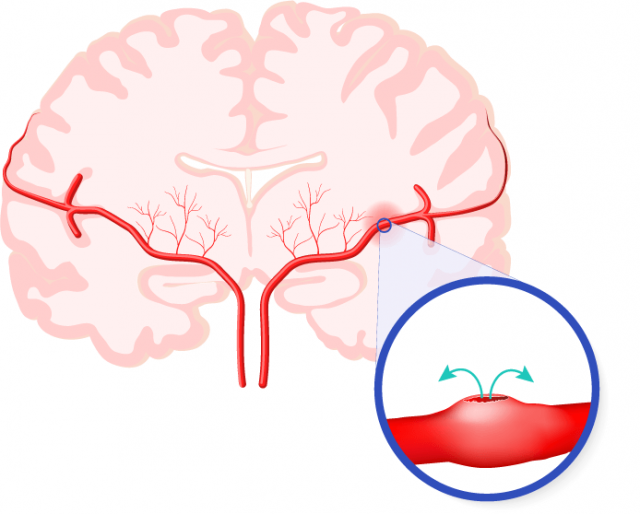
The drug is associated with a higher risk of intracranial hemorrhage. People taking the medication in a study experienced the life-threatening emergency at a rate of 0.22% a year, according to the drug label. In this study, this correlates to one in 454 patients taking Pradaxa over the course of a year.
The risk is highest in people:
- Age 75 and over
- With a stomach ulcer
- With recent or recurrent stomach or intestinal bleeding
- With kidney problems
- With a low body weight
- Who take other medicines that increase the risk of bleeding (aspirin, blood thinners and non-steroidal anti-inflammatory drugs)
- Who take dronedarone or ketoconazole for kidney problems
Antidote Can Reverse Effects in Four Hours
For the first five years Pradaxa was sold in the U.S., there was no way for doctors to stop internal hemorrhaging caused by the drug.
The FDA granted conditional approval for a bleeding antidote in October 2015. The agency gave full approval for the reversal agent Praxbind (idarucizumab) in 2018.
Researchers found that Praxbind reversed the anticoagulant effect of Pradaxa within four hours in the majority of patients.
Praxbind is stocked in more than 3,100 hospitals in all 50 states, according to manufacturer Boehringer Ingelheim. Patients and health care providers can find where the antidote is stocked by using a tool on Praxbind.com.
People allege that Boehringer Ingelheim developed the remedy in 2010 but didn’t seek approval for it until February 2015. Thousands of people who blame Pradaxa for bleeding injuries and deaths have filed lawsuits against the manufacturer.
Spinal/Epidural Hematomas and Stopping Pradaxa
The FDA requires a black box warning — the agency’s strongest warning — to alert the public of the risk of spinal and epidural hematomas in patients treated with Pradaxa who are receiving neuraxial anesthesia or undergoing spinal puncture.
Spinal trauma can also cause these problems in patients taking the drug. In a 2012 case report in the Spine journal, doctors at Seton Brain and Spine Institute at the University Medical Center at Brackenridge in Austin, Texas, describe a 72-year-old man who fell off his roof and suffered back pain and weakness in his legs.
The man had been using dabigatran. In addition to vertebral fractures, he developed an epidural hematoma and cord compression that causes numbness and weakness of his lower extremities. His bleeding was so severe, that doctors had to halt his surgery and operate again seven days later.
Aside from spinal issues, the black box warning also cautions that suddenly stopping the drug increases the risk of blood clot and stroke.
33% Higher Heart Attack Risk than with Warfarin
A March 2012 study found that patients taking Pradaxa were more likely to have heart attacks than those taking warfarin. Researchers analyzed five trials of 30,470 patients. They used information from the U.S. National Institute of Health MEDLINE database. They published their findings in the Journal of the American College of Cardiology.
That same month, a Cleveland Clinic study published in the Archives of Internal Medicine found similar results. The study compared warfarin and Pradaxa. It found that Pradaxa caused a 33 percent increased risk of heart attack or severe symptoms of heart disease. Those symptoms can include chest pain, dizziness, shortness of breath and loss of consciousness.
Calling this number connects you with a Drugwatch representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


