A Patient’s Guide to Telemedicine
Telemedicine allows patients to have a remote, non-emergency office visit with their health care provider by using a smartphone, computer or tablet. Research shows most patients are highly satisfied with telemedicine visits, and in most instances these visits are as good as in-person visits.

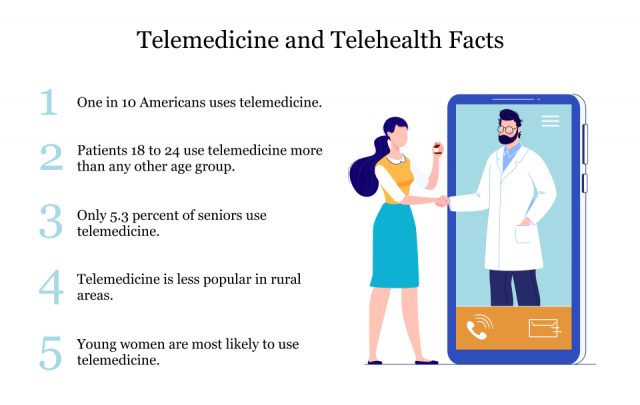
Telemedicine has been growing in popularity in recent years. As more states are implementing laws to facilitate telemedicine, more Americans are embracing remote visits with their health care providers.
From 2016 to 2017, health insurance claims for telemedicine grew by 53 percent, according to FAIR Health’s FH Healthcare Indicators and FH Medical Price Index 2019. Telemedicine claims grew more than claims for urgent care centers, retail clinics and emergency departments.
In 2017, about 76 percent of hospitals in the United States connected with patients and other practitioners virtually through video or other technology, according to the American Hospital Association.
Because of the COVID-19 pandemic, analysts for Forrester Research predicted virtual health care interactions could top one billion by the end of 2020, CNBC reported.

Telemedicine vs. Telehealth
Telemedicine is a component of a larger group of remote health care services called telehealth, though sometimes people use the terms interchangeably.
The main difference between the two is that telemedicine specifically refers to medical information exchanged remotely to improve a patient’s health. Information can be exchanged through email, two-way video, smartphones and other wireless tools.
Telehealth encompasses telemedicine and other types of remote health care information exchanges, such as health education, medical provider training, administrative meetings and more.

Types of Telemedicine
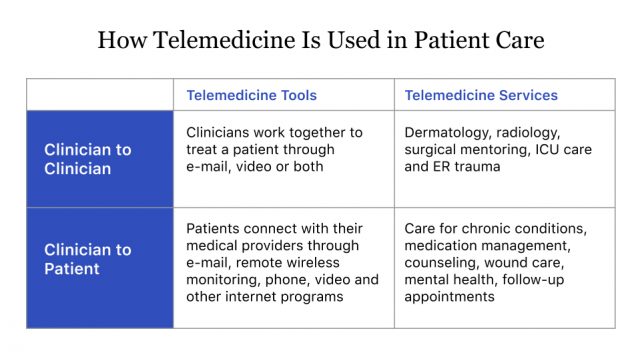
Telemedicine is broken down into three main types of remote clinical services. These are interactive telemedicine, store-and-forward and remote patient monitoring.
Interactive Telemedicine
Interactive telemedicine is also called live telemedicine or real-time telemedicine. Consumers are most familiar with this type of telemedicine. It involves patients and providers communicating directly through video, chat or other remote methods in real time.
This type of telemedicine may take the place of an in-person office visit. It’s popular for urgent care, follow-ups, primary care, managing medications and managing chronic illness.
Store-and-Forward
Store-and-forward telemedicine, also called asynchronous telemedicine, allows patients and providers to transmit medical information for diagnosis or for later review. Examples of information that may be shared from patients to providers and from providers to other providers include lab reports, imaging studies, videos and other diagnostic results.
This type of telemedicine is popular in certain medical specialties such as radiology, ophthalmology and dermatology.
Remote Patient Monitoring
Remote patient monitoring (RPM), sometimes called telemonitoring, uses devices to remotely collect and send data to clinical providers for interpretation. Examples might include blood glucose measurements, heart electrocardiograms (ECG) or other vital sign measurements.
RPM is most often used to monitor patients with chronic illness, high-risk patients or patients recently released from the hospital.

What Can You Use It For?
In some cases, telemedicine can replace in-office visits for regular primary care or specialist consultations or urgent care needs. Specialties that may offer telemedicine services include cardiology, neurology, oncology, gynecology, dermatology, mental health and physical therapy.
Some types of treatment may be better in person, such as biopsies or physical exams. Check with your medical provider to see if you need an in-person appointment.
It’s important to note that people with potentially life-threatening emergencies should seek in-person care.
- Chronic disease management
- Medication management (birth control, chronic illness)
- Non-emergency urgent care (minor injuries, respiratory illness, urinary tract infections)
- Second opinions
- Follow-up visits
- Mental health and addiction counseling
- Primary care visits
- Medical support in assisted living facilities
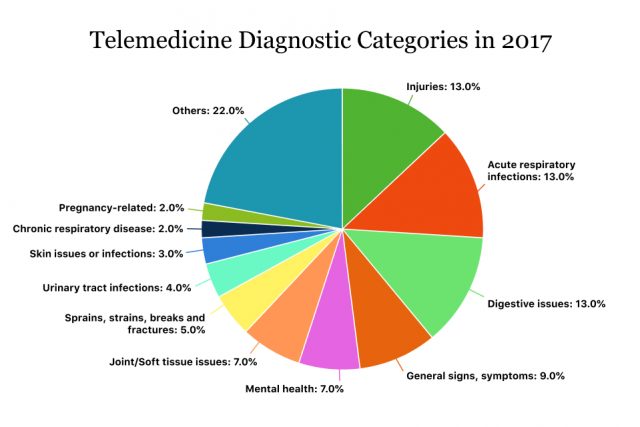
Common Telemedicine Diagnoses
Mental health consultations used to be the number one diagnostic category for telemedicine, according to FAIR Health’s FH Healthcare Indicators and FH Medical Price Index 2019. But in 2017, other telemedicine diagnostic categories such as urgent care injuries surpassed mental health.
COVID-19 Telemedicine Visits
Because of the COVID-19 pandemic, several telemedicine providers, insurance companies and health systems are offering free telehealth consults for anyone experiencing symptoms.
Options for virtual consults vary by state. For example, the South Carolina Department of Health and Environmental Control provides a list of participating providers and a promo code for a free telemedicine consult on its website.
To find out your options, contact your local state health department, your insurance provider or a nearby hospital system.
Can You Get Prescriptions?
Medical providers can prescribe medications through telemedicine.
Normally, telemedicine providers must have at least one in-person visit with a patient before prescribing opioids and other controlled substances. But during the COVID-19 pandemic, the DEA has waived this requirement.
How Much Does It Cost?
The actual out-of-pocket cost of a telemedicine visit varies by insurance provider, but the average cost of a telemedicine visit is less than an in-person visit. Proponents of telemedicine say virtual visits can also save travel time and cost.
According to studies cited by the American Journal of Managed Care, the average cost of a telehealth visit is $40 to $50, while the average estimated cost of in-person care is $136 to $176.
During the coronavirus pandemic, many health insurance companies waived costs for telehealth visits related to COVID-19.
The Coronavirus Preparedness and Response Supplemental Appropriations Act, as signed into law by the president on March 6, 2020, allowed Medicare to cover telemedicine services normally only allowed for in-person visits.

HIPAA Privacy and Security
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) protects health care information shared through telemedicine. Providers are required to use a telemedicine platform that is HIPAA compliant to communicate with patients.
During the COVID-19 pandemic, the Office for Civil Rights (OCR) at the Department of Health and Human Services (HHS) is exercising its enforcement discretion and allowing medical providers to use non-HIPAA compliant software such as Skype or Facetime.
Patients who are concerned about their privacy can ask their medical provider if they use a HIPAA-compliant telemedicine solution. If not, they may look for another provider that does.

Is Telemedicine as Good as an In-Person Visit?
In situations where telemedicine is appropriate, telemedicine visits are typically just as good as in-person visits, according to the American Telemedicine Association (ATA). They may also be less expensive than in-person visits.
The ATA reviewed a large number of telemedicine studies for cost effectiveness and quality of care in its 2013 report, Telemedicine’s Impact on Healthcare Quality and Cost.
“For most telemedicine applications, studies have shown that there is no difference in the ability of the provider to obtain clinical information, make an accurate diagnosis, and develop a treatment plan that produces the same desired clinical outcomes as compared to in-person care when used appropriately,” the ATA said.
A more recent review of studies, performed in 2018, similarly found that in most cases, telemedicine visits were as good as in-person care.
“Being organized with anything that concerns you is even more important when the doctor doesn’t see you in person and can’t notice health issues that might be more obvious in person.”
Eighty-three percent of the time, patients can resolve their health issues during the first telemedicine visit, according to Red Quill Consulting.
One key thing to consider is preparing ahead of time, according to Diana Zuckerman, president of the National Center for Health Research.
“It’s important to make a list in advance of every question and comment before the [telemedicine] doctor’s visit,” Zuckerman told Drugwatch. “Being organized with anything that concerns you is even more important when the doctor doesn’t see you in person and can’t notice health issues that might be more obvious in person.”
Zuckerman advises consumers to write down and keep track of their medical provider’s answers during a telemedicine visit.
| Pros | Cons |
|---|---|
| Patients may save travel and wait time compared to an in-person visit. | You may still need an in-person visit after talking to a provider through telemedicine. |
| You can avoid exposure to germs and other infectious diseases. | In some cases, you may receive better care in person. |
| You can access medical providers even when they aren’t near you, letting you have more choices. | You may not be able to choose the medical provider depending on the telemedicine system you choose. For example, some insurance companies have their own providers that you must use. |
| On average, telemedicine visits cost less than in-person visits. You may also save money by not taking time off work, paying a babysitter or paying for the cost of transportation. | You need a good internet connection and device to access telemedicine. Some people may not have access to internet, and technology might be difficult for older adults to use. |

Getting Started
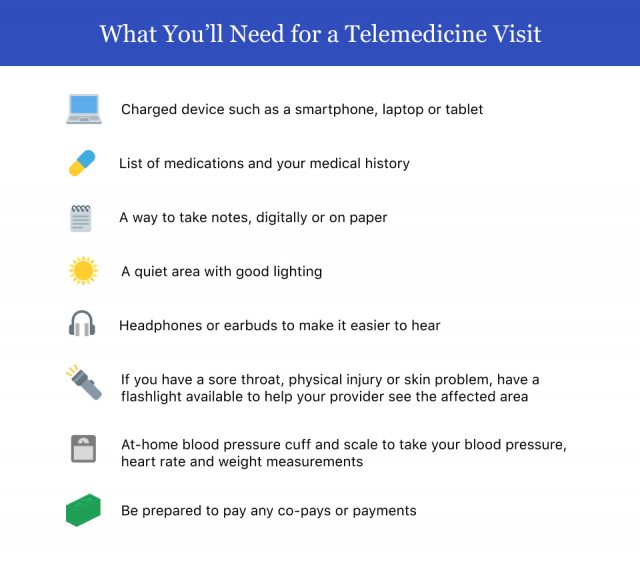
Patients who want to conduct a telemedicine visit with a provider will first need to confirm that the provider offers this option. Second, they will need a reliable internet connection and a smartphone, computer, laptop or tablet.
If you don’t have a preferred medical provider, you can check with your insurance company for providers that participate in their telemedicine program. You’ll also want to check with your insurance company’s policies on paying for these visits.
Ask your HR department if your employer has a preferred telemedicine provider.

Make the Most of Your Telemedicine Visit
Making the most of your telemedicine visit is a lot like making the most of your regular in-person office visits. Planning ahead and having all your information ready will ensure that your visit goes smoothly and that you and your medical provider can communicate properly.
Texas family physician Dr. Karla Dick incorporated telemedicine as a part of her practice because of COVID-19 regulations. She told Drugwatch that she has several tips for patients.
- Have prescription bottles in front of you in case they need to be verified or discussed. Also have your pharmacy information on hand and notify your doctor of any new prescriptions.
- Prepare and have a list of the names and locations of hospitals and specialists that have treated you since your last visit.
- If your provider sends you a link by email or text with a telemedicine how-to video, watch it before your visit. Some providers also have videos and information on their website.
- Make sure you download any apps or create an account on a telemedicine website your provider instructs you to use. Familiarize yourself with the app or website and call your provider with questions before your visit.
- Make sure your device (phone, tablet or laptop) is charged or plugged in.
- Check in to your visit at least ten minutes prior to your appointment time.
- Be patient. The provider is most likely seeing another patient.
- Call your medical provider after your telemedicine visit by phone if you didn’t understand what was discussed or you need to clarify any information.
Calling this number connects you with a Drugwatch representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

