Rheumatoid Arthritis Diagnosis and Tests
People with rheumatoid arthritis (RA) often test positive for a protein called rheumatoid factor (RF) and antibodies called anti-citrullinated protein antibodies (anti-CCP). Other tests, such as erythrocyte sedimentation rate (ESR) and C-reactive protein, can show elevated results in people with RA. Imaging tests may also help doctors diagnose RA.

Diagnosing rheumatoid arthritis early gives the patient a better chance of starting treatment and preventing more serious joint damage. It may also allow a patient to achieve longer periods of remission.
But diagnosing the disease early may be difficult — some symptoms of RA mimic symptoms of other conditions such as gout, osteoarthritis or lupus. Tests may not show RA damage at early stages.
Most people will visit their primary care doctor with symptoms. If the primary care doctor suspects RA, they will usually refer the patient to a rheumatologist. A rheumatologist is a doctor who specializes in RA and other types of arthritis and autoimmune diseases.
The length of time it takes to diagnose RA depends on how many tests a doctor needs to confirm a diagnosis and how long those tests take to return results. Each patient is different.
Confirming a Diagnosis
To confirm a rheumatoid arthritis diagnosis, the doctor will conduct a physical examination and ask about the patient’s medical history. Then the doctor will order lab tests and imaging tests to confirm the physical examination findings.
Physical Examination
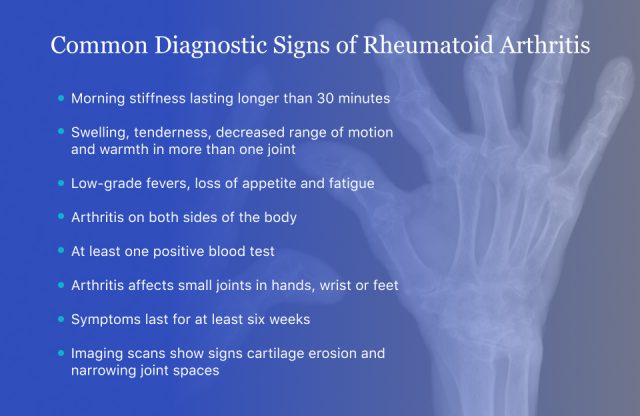
During a physical examination, the doctor will check joints for swelling and pain. These symptoms in RA come with tenderness, redness and warmth in the affected joints, and usually last for more than six weeks.
RA typically attacks smaller joints on both sides of the body — most often the wrists, hands and feet. In some people, it also affects the shoulders, elbows, ankles, hips and knees. People with RA have symptoms in multiple joints. A hallmark of RA is morning stiffness that lasts for more than 30 minutes.
Because RA is an autoimmune disease, it can also cause systemic symptoms such as low-grade fevers and fatigue. It also affects the lungs, eyes, heart, blood vessels and skin.
A physical examination and medical history may lead to a diagnosis of RA even if blood tests are negative.
Blood Tests
During the initial evaluation, the doctor will also order blood tests. These tests search for certain antibodies and markers of inflammation. These tests can confirm the presence of RA and how severe the disease is.
Rheumatoid Factor Test (RF)
A rheumatoid factor test is an antibody test that is positive in people with autoimmune diseases such as RA. The normal range of RF is 0 to 20 units per milliliter (u/ml). An abnormal RF result isn’t enough to diagnose RA since there are other issues that can raise this level, such as other autoimmune diseases, diabetes, bacterial infections and vaccinations.
Anti-Citrullinated Protein Antibody Test (Anti-CCP or ACPA)
Another antibody test for RA is the anti-CCP test. This test is 97 percent specific for RA if the disease is present, according to the Hospital for Special Surgery.
Normal levels of anti-CCP are less than 20 u/ml. Levels higher than 20 suggest the possibility of RA — the higher the test result, the more certain the diagnosis.
About 20 percent of patients test negative for RF and anti-CCP antibodies but may still have a diagnosis of RA based on physical examination and imaging.
Non-specific RA Blood Tests
Two other tests that doctors may use to help diagnose RA are erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). These tests are not specific to RA but they do measure inflammation, which is present in RA. High measurements on these tests indicate how active a patient’s RA is. Other proteins are involved in RA, including sulfatase-2, and tests may be developed for these proteins in the future.
Imaging Tests
In addition to blood tests, a doctor may order imaging tests. These include X-rays, magnetic resonance imaging (MRIs) scans, computerized tomography (CT) scans and ultrasounds. These tests will show the doctor any damage to the joint, cartilage or other tissue damage and inflammation. These tests will also show any bony nodules.
In the early stages of the disease, X-rays may appear normal. MRIs and ultrasounds are more useful for diagnosing RA because they show bone erosion and tissue inflammation, according to the Arthritis Foundation.
Diagnostic Criteria
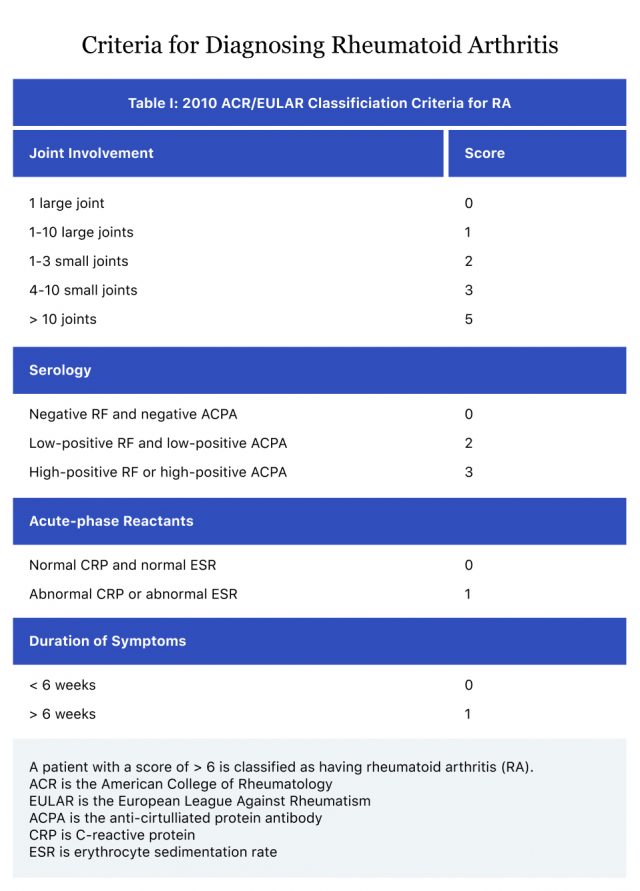
The American College of Rheumatology has a point-based system for diagnosing RA. It has categories based on positive tests, duration of symptoms and number of joints affected. A person must score at least six points to be diagnosed with RA.
Stages of RA
Rheumatoid arthritis is a progressive disease. This means there is no cure, and the goal of treatment is to slow down joint damage and help patients achieve remission. There are four stages of disease, each with worsening symptoms.
Stage One, Early Stage
People with early stage RA start having inflammation in the capsule around joints. Synovial tissue also begins to swell. People feel morning stiffness and discomfort in the joints. Sometimes, moving the joint improves stiffness. Symptoms may come and go, making it difficult to diagnose. At this stage, imaging tests may pick up evidence of osteoporosis.
Stage Two, Moderate
During stage two, antibodies will be more likely to show up in tests and swelling worsens. There is slight or no bone damage. People may start to develop nodules on the elbows and other joints. At this stage, MRIs are more likely to pick up joint damage than X-rays. RA is easier to diagnose during the second stage.
Stage Three, Severe
The disease becomes severe at stage three. Cartilage and bone damage are present. Swelling, pain and stiffness in tissues become severe and muscle starts to atrophy. At this stage, joints may become deformed and bent. This causes nerve pain from pinched nerves.
Stage Four, End Stage
End stage RA is the most severe form of disease and the cartilage is completely gone. People at this stage lose the ability to move a joint because the joints may fuse together. Fortunately, many treatments are available to help keep the disease from getting to this stage.
Progressive Rheumatoid Arthritis
People whose disease continues to get worse and advance through disease stages have progressive rheumatoid arthritis. As the disease progresses through the stages, inflammation and pain worsen and flare-ups become more frequent. Other symptoms that affect other parts of the body may also start.
Progressive rheumatoid arthritis requires a more tailored, intensive treatment plan to slow disease progression.
- The disease is active more frequently
- Flare-ups become more regular and last longer
- Swelling and pain spread throughout the body and become more intense
- More nodules develop in joints
- Measurements of RF and anti-CCP show higher levels
Differential Diagnoses
RA is difficult to diagnose because it shares symptoms with a few other types of diseases. Doctors use a combination of blood and imaging tests to rule out these other conditions.
- Fibromyalgia, a condition with widespread musculoskeletal pain, fatigue and mood issues
- Lyme disease, a bacterial infection cause by the bite of an infected tick
- Myelodysplastic syndrome, a condition that occurs from poorly formed blood cells
- Paraneoplastic syndromes, conditions triggered by a disordered immune system response to cancer
- Relapsing polychondritis, a rare condition that causes inflammation in cartilage and tissues in the body
- Polymyalgia rheumatica, an inflammatory disorder that causes stiffness and muscle pain, usually in the shoulders
- Other types of arthritis, such as osteoarthritis and psoriatic arthritis
- Sarcoidosis, inflammatory disease that affects multiple organs
- Sjogren’s syndrome, an autoimmune disorder that affects tear ducts and salivary glands
- Lupus, also called systemic lupus erythematosus (SLE), an immune disorder where the body attacks healthy tissues and organs
Calling this number connects you with a Drugwatch representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

