Managing Pain after Surgery
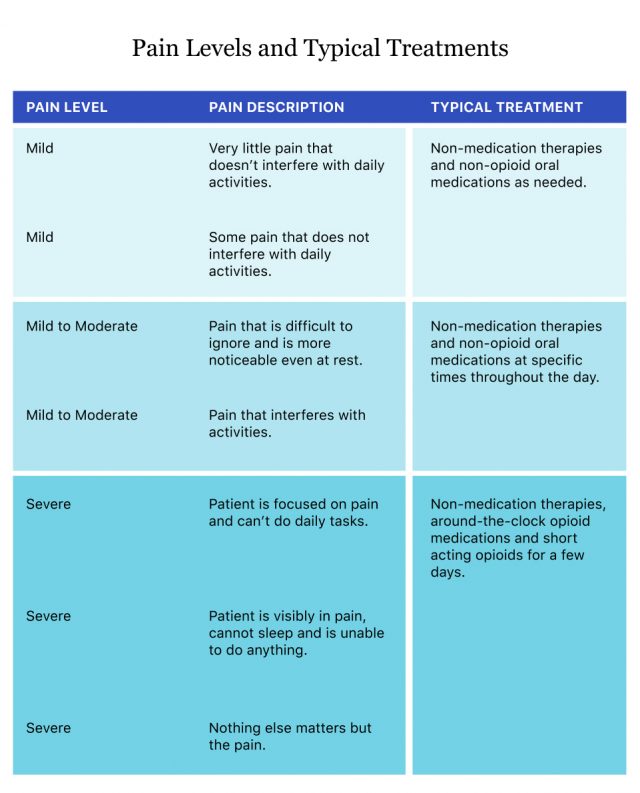
Effectively managing pain after surgery can help avoid complications, speed up healing and keep patients moving. Depending on the type of surgery, patients may experience different pain symptoms such as sore muscles, nerve pain or swelling. Treatments for managing pain after surgery include oral and injectable medications and non-pharmacological options such as meditation and acupuncture.

The goal of effective post-operative pain relief is to eliminate or reduce pain with minimum side effects.
Researchers found that effective pain relief leads to better health outcomes such as reduced hospital stays, reduced hospital costs and better patient satisfaction, according to Drs. Veerabhadram Garimella and Christina Cellini at the University of Rochester Medical Center in New York.
Managing pain after surgery can also help avoid complications such as tachycardia (irregular heartbeat), hyperventilation, decreased oxygen in the body (alveolar ventilation), poor wound healing, insomnia and chronic pain.
As a patient, you work with your provider to control post-op pain. This means making sure you understand and follow the pain management plan your provider has given you.
If you don’t understand pain management instructions or you feel pain, it’s important to let your provider know.
“In general, the line of communication should always be open. There’s no reason for patients to be stoic,” Dr. Hooman Noorchashm, a general and cardiothoracic surgeon who has practiced at Thomas Jefferson University Hospital and Brigham and Women’s Hospital, told Drugwatch. “The doctors are there to listen to their problems and to resolve their problems.”

Types of Pain You May Feel after Surgery
The severity and type of pain you feel depends on the type of surgery. For example, major surgeries like thoracic surgery or hip replacement will typically require stronger pain medications for a month or more. But the pain from less invasive surgeries like gallbladder removal may only last a few days.
More than 80 percent of patients who have surgery suffer from acute post-op pain, according to an American Pain Society study led by Dr. Roger Chou of Oregon Health and Science University.
“Not every surgery is created equal and not every big incision is as painful as some smaller incisions. So, if you make an incision on someone’s rib cage, it is very different than an incision that you make on someone’s abdomen or on someone’s sternum,” Noorchashm said.
- Muscle pain in the neck, shoulders, back or chest from spending time on the operating table
- Sore and scratchy throat because of the breathing tube
- Pain when walking, sitting up or coughing.
Hernia Mesh Surgery
After hernia mesh surgery, patients will feel soreness, numbness or tenderness at the incision site that lasts for a few weeks.
If doctors used mesh, patients might feel discomfort for up to 6 months. Symptoms specific to hernia surgery include a feeling of “pulling” at the surgery site, tingling and difficulty sleeping, walking or sitting.
If the patient had laparoscopic surgery, they may have left shoulder pain caused by the gas pumped into the abdomen during surgery. This may last for a day or two.
Knee Replacement
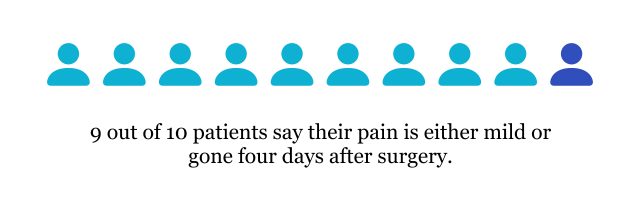
After knee replacement surgery, patients will feel soreness and swelling at the surgery site. Patients reported that post-operative pain was “aching, heavy and tender,” according to researchers V. Wylde and colleagues. Night pain disturbed about half of the patients in the study for up to three nights after the surgery.
In a study by researchers E.Y. Chan and colleagues from the University of Sydney in Australia, patients reported that the worst pain occurred during the first two weeks. The study also reported that patients had inadequate instructions when they were discharged from the hospital.
This makes it more important for patients to ask questions before they go home.
Hip Replacement
After hip replacement surgery, patients may feel some numbness or pain in their thighs along with swelling, soreness and bruising at the incision site. This happens because of nerve fibers the surgeon cuts during surgery. Typically, this sensation subsides over time.
There will be pain after surgery, but doctors recommend patients start moving as soon as possible with physical therapy, according to the University of Missouri. Doctors will prescribe pain medications to decrease pain felt during therapy.
“The first surgery pain only lasted for 60 days, same as second surgery. It was really high for pain for the first two weeks.”
It is most severe in the first few days following surgery, but hip replacements are major surgeries and the pain can last for a couple of months.
“The first surgery pain only lasted for 60 days, same as second surgery,” hip replacement patient Don Dupuis told Drugwatch. “It was really high for pain for the first two weeks, and both I was off work for three months.”
Dupuis ended up suffering from metal poisoning called metallosis because of his metal-on-metal hip implant and had to have more surgeries. Now, he is on pain medication for the rest of his life.

Medications for Controlling Pain
The American College of Surgeons breaks down the medication options for controlling pain into two main categories: non-opioid oral medications and opioids. Most pain management plans involve one or both of these.
The patient and surgeon will work together to create a plan. The surgeon may also consult a pain specialist. It’s important that patients tell providers about all medicines they take, including herbal supplements and vitamins.
In general, Noorchashm says the worst post-op pain occurs within 48 to 72 hours, and pain that requires narcotic pain relief may last from five to 14 days after surgery.
“During that period is when we would rely on the devices called patient controlled anesthesia [PCA] which is like a button the patient pushes to deliver an IV narcotic like Dilaudid or morphine,” he said. “Then after that, depending on whether the patient can take pills, you sort of revert patients back to oral forms of the medication.”
There are pros and cons to most medications, including serious side effects. This is especially true of opioid medications, which are very addictive.
| Drug | Side Effects |
|---|---|
| Tylenol (acetaminophen) for fever and pain. | Common: Headache, insomnia, nausea, vomiting. Serious: Higher doses may cause liver damage, don’t exceed 4,000 mg in 24 hours. |
Non-steroidal anti-inflammatory drugs (NSAIDs) for swelling and fever:
| Common: Stomach upset, gas, bloating, nausea, vomiting
Serious: Gastrointestinal bleeding, increased risk of heart attack and stroke |
Drugs that reduce nerve pain:
| Common: Drowsiness, dizziness, memory loss, lack of coordination, difficulty speaking, anxiety, depression, infection Serious: Suicidal behavior and ideation, sudden unexplained death in epilepsy patients, anaphylaxis and angioedema |
| Drug | Side Effects |
|---|---|
Opioids:
| Common: Constipation, nausea, dizziness, dry mouth, drowsiness, itching, slow breathing, vomiting, itching
Serious: Overdose, misuse, addiction, death from respiratory depression (slow breathing). Risk of addiction increases the longer a patient takes the drug. Patients at risk of addiction will have a special postoperative pain plan. |
Patient-Controlled Analgesia (PCA)
Right after surgery, patients may receive medications through an IV line connected to a pump. The patient can press a button when they feel the need for more medication and the pump will deliver it.
The pump is set to make sure patients cannot give themselves too much medicine. The important thing about PCA is that the patient presses the button and is awake enough to know they need medication.
Doctors may decide to place the PCA tube through the back. This is patient-controlled epidural analgesia. For some patients, this may be more effective than a typical IV line.
Nerve Blocks
Nerve blocks control pain in a smaller, specific area of the body such as a leg or arm. An advantage to this type of pain relief is that smaller, more controlled doses of opioids may be used and can lower the risk of side effects.
Your Role in Pain Control
Your main role as a patient is to make sure you tell your surgical team or health care provider if you have pain. Also, make sure to take your medication at the scheduled time and don’t wait until you are in pain to take your medication.
Donna Wagner, a double bypass patient, made the mistake of not taking her medications regularly. She said it was a lesson she had to learn the hard way.
“When I came home [from surgery], I thought, ‘I am not going to take as much pain medicine.’ So I cut back on the pain medicine,” Wagner told Drugwatch. “The second night I was home I was sitting, and I just didn’t feel well, and my whole left arm and shoulder got really sore and heavy. It scared me a little.”
Make sure you understand how to wean off stronger medications and don’t just stop taking them.

Using Opioid Pain Killers Safely
Providers commonly prescribe opioids, also called narcotics, after surgery. While they are effective at controlling pain, they are also highly addictive. People who take them for a long time also build up a tolerance to them.
Withdrawal symptoms from opioids include anxiety, racing heartbeat, insomnia and headaches. After using these drugs for five days, the risk of addiction increases, and the longer a person takes them, the greater the risk.
“In general my own strategy has always been to try and minimize the amount of narcotics used and to revert patients to an ibuprofen, Tylenol-type regimen as quickly as possible,” Noorchashm said. “For a routine abdominal operation [like hernia surgery], that would probably take up to 5 to 10 days where I could reliably wean someone.”
Patients may also wait to fill their opioid medications and try non-opioids with the permission of their provider, and the prescription is good for up to 7 days after your provider issued it.
According to the American College of Surgeons, 400 mg of ibuprofen provided as much pain relief as 5 mg of oxycodone for patients with abdominal or pelvic surgery.
- Don’t take more medication than prescribed and don’t crush pills.
- Take the lowest dose possible.
- Don’t share opioids.
- Don’t take opioids with drugs that cause drowsiness such as sleep aids, antihistamines, anti-anxiety medications muscle relaxers or other opioids unless told to by your provider.
- Don’t take opioids with alcohol.
- Opioid overdose is deadly. Call 911 if the patient suffers symptoms of overdose such as trouble breathing, small pupils or unconsciousness.
Ways to Control Pain without Medications
Providers may recommend patients use non-medication pain relief therapies for mild postoperative pain. These therapies include massage, acupuncture and hot and cold therapy.
In fact, something as simple as walking can speed up healing. It also prevents complications such as blood clots.
“After every surgery I was told to walk around every day to keep active, not become a couch potato,” said hip replacement patient Dupuis.
| Therapy | Examples |
|---|---|
| Complimentary therapy | Meditation, acupuncture, massage, music, guided imagery |
| Self-care | Rest, ice and elevation |
| Rehabilitation | Physical and occupational therapy |
| Exercises | Mild exercise such as walking and stretching |
Orlando-based Licensed Acupuncture Physician and Diplomate of Oriental Medicine Samadhi Artemisa treats patients holistically for pain with a combination of diet, massage and acupuncture.
A key element of pain is inflammation.
“The first thing that I recommend is to eliminate a group of foods that are inflammatory. They are commonly referred to as nightshades,” Artemisa told Drugwatch. “Avoiding these is not going to reduce somebody’s pain but it will make it so it’s not worse.”
Nightshades include potatoes (except sweet potatoes), peppers (except black pepper), tomatoes, eggplant, goji berries and paprika. Always check with your doctor when making dietary changes or taking supplements.
One of the most powerful anti-inflammatory foods is ginger, Artemisa said. She recommends making ginger tea out of fresh ginger, which is more medicinal than teas that come in tea bags.

“Once [patients] are clear for getting treatment, massage or acupuncture is very helpful. Especially around an incision,” Artemisa said. “There is a technique that we use in acupuncture that’s called Surround the Dragon. That’s amazing for helping the incision to heal and close more quickly and can keep scar tissue from forming.”
Meditation and rest are equally helpful and important, Artemisa adds.
“So frequently people just want to jump back into their daily routine. But rest is really, really valuable for the body to be able to repair itself,” she said.

Questions to Ask Your Provider
The line of communication between provider and patient should always remain open. Before talking to your provider, make sure you write down a list of questions and concerns. Bring it with you to the appointment.
If you think you might have difficulty understanding your doctor’s answers, don’t be afraid to bring a friend, family member or professional patient advocate.
For surgeries like hip or knee surgeries, patients may have to be on narcotic painkillers for more than a month. Noorchashm recommends patients ask about opioid medications, specifically.
“You’re talking about having a physician that doesn’t just write a blank check for patients on narcotics but is actually thoughtfully looking at how to wean them off as quickly and safely as possible,” he said.
- What kind of pain can I expect?
- About how long will the pain last?
- How do you personalize narcotic needs?
- What are you going to do to wean me off narcotics as quickly as possible?
- What time frame do you think I’ll be dependent on narcotics?
- How addictive are these narcotics?
- What happens if I have difficulty weaning off these narcotics?
- What is your plan for withdrawal symptoms I may have?
- Can I avoid long-acting narcotics like OxyContin?
- What is your protocol for opioid dependency and withdrawals?
Most importantly, Noorchashm tells patients to speak up.
“It’s important that patients always communicate with their practitioner when they are in a lot of pain. There is no hard and fast rule about what level of pain is too much pain,” he said. “If you are in pain and you feel like you need to talk to someone about that pain, you need to talk to someone.”
Calling this number connects you with a Drugwatch representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


