What is a Urogynecologist?
A urogynecologist is an OB-GYN with advanced training and expertise in the treatment of pelvic floor dysfunction in women. Women with complex pelvic floor problems are usually referred to urogynecologists by their primary care doctor or OB-GYN. Urogynecologists can prescribe nonsurgical treatments, such as medication or pelvic exercise, and surgical treatments, such as implanting transvaginal mesh, which can cause complications.
Urogynecology is a fairly new subspecialty of gynecology, but it’s growing fast. Increasing rates of pelvic floor disorders have raised the demand for specialized services. The pelvic floor is a structure composed of muscles, ligaments, nerves and connective tissues that support pelvic organs and assist in the control of their functions.
In the 1970s and ‘80s, most gynecologists could treat pelvic floor disorders. But as gynecologists began to see more women for primary needs, they received less specialized training on pelvic floor issues.
The American Board of Obstetricians and Gynecologists and the American Board of Urology established the Female Pelvic Medicine and Reconstructive Surgery certification. An FPMRS certification is the highest level of accreditation for urogynecologists.
In 1996, there was one board-accredited fellowship program for advanced training in urogynecology. By June 2010, the number of accredited fellowship programs had grown to 37, and membership in societies associated with the sub-specialty had doubled, according to the American Journal of Obstetrics and Gynecology.
People see urogynecologists to treat conditions such as:
- Lower abdominal pain
- Sphincter issues
- Bladder problems
- Pelvic organ prolapse
- Stress urinary incontinence
- Transvaginal mesh complications
OB-GYNs can still provide routine care for women with simple pelvic floor issues. But they often refer women to urogynecologists for the assessment and treatment of complex pelvic floor problems.
Training to Become a Urogynecologist
A urogynecologist is a physician who has completed medical school and a four-year residency in obstetrics and gynecology. They may go on to receive additional, highly specialized training in surgical and nonsurgical treatment of pelvic floor disorders. However, that level of training is not required to become a urogynecologist.
After residency, they may complete a fellowship to become specialists in the evaluation and treatment of health conditions that affect women’s pelvic organs such as the vagina, uterus, rectum and bladder.
Once they’ve completed their fellowship, urogynecologists must pass an exam to become FPMRS certified. By the time they become FPMRS certified, urogynecologists have received at least seven years of training after medical school.
Pelvic Floor Disorders
Pelvic floor disorders occur when the pelvic floor is weakened or stretched by childbirth, obesity, surgery, disease or activities such as high-impact sports or repetitive heavy lifting. Pelvic floor disorders can cause urinary or fecal incontinence, pelvic or vaginal pain, difficulty emptying the bladder or bowels, and pelvic organ prolapse. Pelvic organ prolapse is the dropping of pelvic organs from their normal position.
Depending on the severity of symptoms and the health of the patient, nonsurgical therapies are often the first approach in the treatment of pelvic floor disorders.
Nonsurgical treatments for pelvic floor disorders include:
- Medication
- Pelvic muscle exercise
- Lifestyle and dietary modifications
- A vaginal support device called a pessary
- Biofeedback and electric stimulation of pelvic floor muscles
Primary care physicians and gynecologists rarely recommend these treatments. They often refer patients to a urogynecologist for surgical or nonsurgical treatment.
If nonsurgical treatments fail to provide adequate symptom improvement, surgery may be used to repair pelvic floor defects. Urogynecologists with an FPMRS certification are the most qualified doctors for performing this surgery, but other surgeons may also be qualified to perform surgery to treat pelvic floor disorders.
Patients considering surgery should ask their urogynecologist about alternatives to transvaginal mesh for treating prolapse. In October 2022, the FDA reaffirmed its stance that the benefits of mesh placed transvaginally for prolapse do not outweigh the risks.
How Urogynecologists Help with Transvaginal Mesh Complications
Transvaginal mesh is intended to be a permanent surgical implant. The body’s tissues grow into and around the implant. Thus, it can be difficult to remove. But removal of the transvaginal mesh implant is necessary to restore health and quality of life for most women. Urogynecologists are the most qualified physicians to perform mesh revision procedures.
Transvaginal mesh implants have been widely used to repair pelvic floor disorders during the past decade. However, these synthetic mesh implants have caused complications in a significant number of patients.
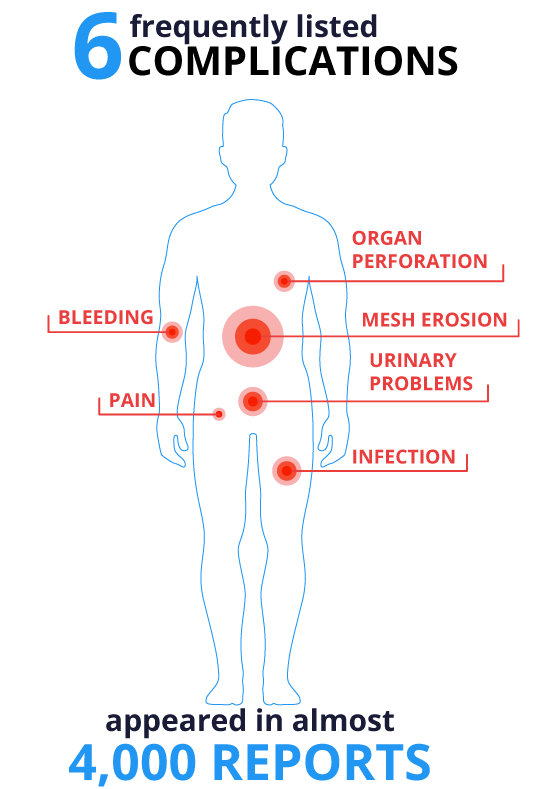
The U.S. Food and Drug Administration received almost 4,000 adverse event reports associated with transvaginal mesh procedures in the five years between 2005 and 2010. The most frequently reported complications included mesh erosion, pain, bleeding, infection, organ perforation and urinary problems.
Mesh contraction was also reported, as well as neuromuscular problems, vaginal scarring and shrinkage, recurrent prolapse and sexual dysfunction. Many urogynecologists avoid mesh products today.
How to Find a Urogynecologist
If you need to find a urogynecologist in your area for pelvic floor problems or transvaginal mesh-related complications, ask for a referral from your OB-GYN or family doctor. If they are not able to help, call university hospitals in your area. University hospitals often have urogynecologists on staff or they can offer recommendations.
You can also contact your insurance provider to see which urogynecologists are covered by your insurance plan.
The American Urogynecologic Society website also provides listings that can help you find credentialed urogynecologists in your area.
Many women who experienced complications caused by transvaginal mesh filed lawsuits against the makers to seek compensation for their injuries. If you are involved in a transvaginal mesh lawsuit, your lawyer may be able to recommend a urogynecologist who has experience in treating problems associated with transvaginal mesh.
With proper treatment, urogynecologists can help women suffering from pelvic floor disorders or transvaginal mesh complications recover from their ailments.
Calling this number connects you with a Drugwatch representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

