Hysterectomy: Removal of the Uterus
A hysterectomy is a surgical operation to take out a woman’s uterus. Doctors perform the surgery to treat several health problems, including uterine fibroids, cancer and prolapse. Hysterectomies are major surgeries with several risks, but most women do not experience complications.
A hysterectomy is a surgery for the removal of a woman’s uterus, also called the womb. This stops a woman’s menstrual cycle and ability to become pregnant. The surgery is more common in the U.S. than anywhere else in the world.
According to the Centers for Disease Control and Prevention, 600,000 women undergo the procedure each year and about 20 million American women have already had it done — making this surgery the second most frequently performed procedure for women in the U.S.
In some cases, this surgery is life-saving and necessary to improve a woman’s quality of life. For instance, women who have uterine cancer or painful uterine fibroids may need to have their uterus removed to improve survival or relieve painful symptoms. Others who have complications from implants such as the Essure Permanent Birth Control may be forced to remove their uterus and fallopian tubes because of extensive damage caused by metal coils in the device.
However, sometimes women have unnecessary hysterectomies that put them at increased risk for a number of other health problems. Complications include hormone imbalance and pelvic organ prolapse, a condition that leads to pelvic organs sagging into the vagina.
Some surgical techniques may put women at risk for future complications. Procedures performed with a surgical tool called a power morcellator may put women at risk for spreading undiagnosed uterine cancer in the abdominal cavity. If transvaginal mesh is used during a hysterectomy, it could erode or perforate organs, causing severe pain and requiring additional surgery.
A study published in the American Journal of Obstetrics and Gynecology in March 2015 questioned the number of hysterectomies performed in the U.S.
For instance, a number of women had their uterus removed for abnormal uterine bleeding when there were alternative therapies that doctors could have tried before surgery.
Before a woman undergoes a hysterectomy, there are a number of factors to consider, including the type of procedure about to be performed, the surgical technique a doctor may recommend and the possible complications.
Hysterectomy Complications
Regardless of the type of surgery used, a hysterectomy is considered a major surgical procedure with the possibility of several complications. Major complications are rare, but serious. More experienced surgeons typically have less trouble with complications. Some complications are common, such as infections and bleeding.
Women are usually less aware of other complications, such as the threat of uterine cancer, pelvic organ prolapse or incontinence. The overall rate of these complications is about 1 percent, but some complications can be fatal.
- Infection
- Infections usually occur in the incision or the top of the vagina, also called the vaginal cuff. While infections usually respond to antibiotics, sometimes more surgery is needed to treat the infection. Patients typically have a 30 percent chance of infection while at the hospital, making it one of the most common complications of hysterectomies.
- Pain
- About 85 percent of women suffer moderate-to-severe pain after surgery that necessitates pain medication. Some women may have to take highly addictive drugs, such as morphine or fentanyl, for relief.
- Blood Loss
- The average blood lost during a hysterectomy is roughly the same amount as three menstrual cycles. During an abdominal hysterectomy, it is double that. Women should be aware that a blood transfusion may be necessary.
- Organ Damage
- The organs surrounding the uterus may be damaged during surgery. For example, the bowel, bladder and urinary tract may be injured. If the bowel is injured, it can be especially troublesome because infection sets in quickly after a bowel injury. Surgeons try to catch injuries during surgery so they can repair the damage.
- Early Onset Menopause
- Even if a woman retains her ovaries, menopause can come 4 to 5 years earlier in women who have had their uterus removed. Without the uterus, blood flow to the ovaries might be disrupted, preventing them from properly producing hormones.
- Psychological Problems
- A number of mental changes may occur after a hysterectomy. Some studies found women experience depression, anxiety and decreased sex drive after the operation. Some women may need to take medications to control the symptoms.
- Increased Risk of Heart Attack and Stroke
- If a woman has the procedure done before her 50s, she is at increased risk of heart attack and stroke.
- Urinary or Fecal Incontinence
- Frequent urination, incontinence and bowel dysfunctions can also occur, leaving a woman constipated or with fecal incontinence.
- Pelvic Organ Prolapse
- Without the uterus, pelvic organs may sag into the vagina, a condition known as pelvic organ prolapse. This may require more surgery to repair. Some women may have transvaginal mesh implanted to hold up sagging organs. But these implants carry complications of their own, such as organ perforation and painful sex. Women who have suffered transvaginal mesh complications have filed lawsuits against companies that made the devices.
- Increased Risk of Cancer
- Some studies connect hysterectomies to several cancers, including thyroid cancer, bladder cancer and renal cancer.
- Risk of Spreading Uterine Cancer
- Certain surgical techniques may increase the risk of spreading uterine cancer. Cancerous cells can hide in fibroids and other tissues. Without testing fibroids before surgery, it is impossible to tell if cancerous cells are present. A number of women have received surgery with a tool called a power morcellator, a drill-like device that chops up fibroids and uterus tissues into smaller pieces for easy removal but also puts them at risk for spreading of cancer cells. Some women have gone in for a routine operation and come out with stage 3 or 4 uterine cancer.
These are just some of the complications that can occur. Depending on any other health issues a woman may have, she may be at risk for additional complications.
When Do Doctors Recommend Hysterectomies?
The U.S. Food and Drug Administration’s Office on Women’s Health suggests that a doctor may recommend a hysterectomy in a handful of cases. Keep in mind that there may be alternatives to this surgery even with these conditions. Women should always discuss all options with their doctors.
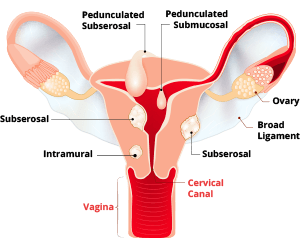
Uterine Fibroids
Uterine fibroids are benign, noncancerous masses of tissue that grow on the walls of the uterus. For some women, fibroids do not pose much of a problem without treatment. However, some women may suffer pain, discomfort or heavy bleeding. If there are too many fibroids to remove individually, a doctor may recommend removing the uterus. Fibroids are the most common reason women get hysterectomies.
Uterine Prolapse
After several vaginal births, a woman may suffer uterine prolapse — a condition where the uterus slips out of its usual place in the pelvic cavity and sags into the vagina. Obesity and menopause may also cause this problem. If the uterus sinks into the vagina, this can cause bowel and urinary problems, as well as pelvic pain and discomfort, so a hysterectomy may be recommended to address this.
Endometriosis and Adenomyosis

Endometriosis occurs when the lining of the uterus grows outside of the uterus. This can cause heavy periods and pain. Adenomyosis occurs when the lining of the uterus grows inside the wall of the uterus, making the wall overly thick. This causes severe pain and heavy bleeding. In both cases, a hysterectomy may be recommended or indicated.
Cancer
If cancer is present in the ovaries, uterus, cervix or lining of the uterus, a hysterectomy may be the best option for treatment.
Different Types of Hysterectomies
There are three different types of hysterectomies, depending on the amount of the uterus removed.
- Total Hysterectomies
- The most common type of hysterectomy, it removes the entire uterus, including the cervix. Doctors may or may not remove the fallopian tubes and ovaries as part of this procedure.
- Partial Hysterectomies
- Removes the upper part of the uterus and leaves the cervix in place. As with a total hysterectomy, the ovaries may or may not be removed.
- Radical Hysterectomies
- Most often used to treat cervical or other cancers. This procedure removes all of the uterus, the cervix and tissue surrounding the cervix, including part of the vagina. The ovaries and fallopian tubes may or may not be removed.
Some women are not counseled about the differences between total and partial hysterectomies. Doctors may remove the cervix as a precaution without informing the patient.
How is a Hysterectomy Performed?
Depending on the woman’s health history and reason for surgery, a surgeon will decide on the best type of technique. Each of these has risks and benefits.
Abdominal

In this technique, doctors make a cut about 15 cm in length in the lower abdomen to reach the uterus. One of the drawbacks to this technique is lengthy recovery and a lot of blood loss, but it is the most popular technique performed in the U.S. Surgeons must cut through several layers of fat and muscle and the lining of the abdominal cavity.
Most abdominal hysterectomies are also called total abdominal hysterectomies because doctors choose to remove the cervix and the uterus. Some doctors argue that the cervix should be left in place because its removal may cause problems later on. But studies show that women who keep the cervix may still have a 20 percent chance of spotting. Because of the extensive tissue cutting involved, it takes about 6 to 8 weeks to recover.
Vaginal

Doctors access the cervix and uterus through a small cut in the vagina. After gently cutting the uterus away from surrounding tissues, the surgeon can pull the tissue out through the vagina. The top of the vagina is sutured with sutures that dissolve on their own in 4 to 6 weeks.
There is less pain and no scar on the stomach with a vaginal hysterectomy. Women also recover more quickly from this type of hysterectomy. It generally costs less to perform, but the organs are less visible and doctors may have a more difficult time seeing them during surgery.
Laparoscopic

With advances in surgical technique, many doctors are in favor of a laparoscopic approach, possibly utilizing a robot to allow the doctor to manipulate the instruments. Studies show that this approach leads to less bleeding, less pain and less risk of infection. Many doctors recommend this type of surgery to women who cannot have vaginal hysterectomies.
Doctors insert a laparoscope with a small camera at the end along with several tools through small incisions in the abdomen. Doctors use a monitor to see the inside of the pelvis and make the necessary cuts. Many surgeons use thermal energy to seal blood vessels and cut tissues.
Surgeons can then pull the uterus out of the vagina or through a small incision in the abdominal wall. Women usually recover in about 3 weeks, and patients are usually able to go home the day of surgery.
Some surgeons use a tool called a power morcellator during a laparoscopic hysterectomy. These instruments resemble drills that have long tubes with cutting blades at the end. Surgeons use these devices to chop up pieces of fibroids or chunks of the uterus and suck them out of the pelvic cavity through a small tube. But the FDA has warned that power morcellators may spread undiagnosed uterine cancer that may be hiding in fibroids or other tissues.
If you are considering having a hysterectomy, it is very important that you ask your doctor if he or she will be using a power morcellator.
V-NOTES Surgery
Transvaginal natural orifice transluminal endoscopic surgery, or V-NOTES, is a new hysterectomy technique that combines traditional laparoscopic surgery with vaginal surgery. Proponents of this surgery say it leads to better outcomes and recovery for patients.
A January 2022 study in Journal of Minimally Invasive Genecology found “hysterectomy by V-NOTES can be performed as a safe and adequate alternative to VH.” Fewer patients had hospital-readmission in the V-NOTES group.
Alternatives
There are a number of other treatments that may be able to address certain conditions without removing the uterus. Make sure you have an in depth conversation with your doctor about your options.
- Uterine prolapse
- Instead of removing the uterus, a woman may be able to do Kegel exercises and other pelvic floor therapies that strengthen the pelvic muscles.
- Endometriosis
- Removal of the endometrial tissue while leaving the uterus intact or oral contraceptives.
- LEEP procedure
- If precancerous or abnormal cells are in surface tissues or are very light, doctors may be able to do a loop electrosurgical excision procedure. LEEP removes these problematic cells.
- Abnormal bleeding
- Several things may cause abnormal bleeding, including hormone levels, infection, fibroids or cancer. Some treatments include dilation and curettage, where the lining and contents of the uterus are removed. Medications, hormones and IUDs may be used to treat these conditions without surgery.
- Restricting blood flow
- Doctors may be able to cut off the blood supply to a fibroid and stop it from growing without removing the entire uterus. Fibroids may also be removed in a procedure called a myomectomy.
As always, patients have the right to a second or third opinion. Before undergoing a major surgery like a hysterectomy, make sure to weigh all the risks and benefits and discuss them with your doctor.
Some Hysterectomies Are Unnecessary
According to some studies, hysterectomies are often overused for benign conditions that may not warrant them.
“For 81 percent of hospitals, at least half of all hysterectomies performed between 2015 and 2017 were unnecessary. 1,167 hospitals performed at least 20 unnecessary hysterectomies between 2015 and 2017, and 495 hospitals performed at least 50,” according to the Lown Institute.
Conditions where a hysterectomy might not be necessary include: Benign uterine fibroids, abnormal pelvic bleeding, pelvic pain and a painful bladder condition called interstitial cystitis.
Hysterectomy and Interstitial Cystitis
Interstitial cystitis symptoms such as pelvic pain and urinary urgency may overlap with other conditions and make IC difficult to diagnose. Because of this, women with undiagnosed IC may have unnecessary hysterectomies, according to Drs. Maurice K. Chung and Barry Jarnagin.
Hysterectomy is a major operation with several potential complications. In contrast, a patient may be able to control IC symptoms with a medication called Elmiron.
Elmiron side effects are typically mild and include: Hair loss, gastrointestinal upset and nausea. However, recent studies have linked Elmiron to a type of eye damage called pigmentary maculopathy that could lead to permanent vision loss.
Before having a hysterectomy, patients should ask their doctors to rule out IC.
Calling this number connects you with a Drugwatch representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


